The was a phased opening with three operating theatres. The centre moved to full capacity with five operating theatres in May 2024.
Patients referred to any hospital in north west London for routine inpatient orthopaedic surgery who are generally in good health may now have their surgery in the new ‘elective orthopaedic centre’. Over 4,000 patients a year are expected to have their surgery at the new centre once it is at full capacity.
The centre focuses on routine surgery, primarily hip and knee replacements, for patients who are otherwise well. Each patient’s care is overseen by the consultant from their local hospital, who joins them at the centre to do the surgery on the day. The rest of their care – before and after surgery – takes place at their local hospital, in their community, or online at home. The centre, and its permanent specialist team, are managed by London North West University Healthcare.
The centre has five operating theatres. Patients from Imperial College Healthcare, Chelsea and Westminster, The Hillingdon Hospitals, and London North West University Healthcare, are now able to have their surgery at the centre.
Care pathways for patients with complex health needs and day-case patients are unchanged and surgery is provided at a range of north west London hospitals. These patients also benefit from shorter waiting times, as moving low-complexity, inpatient surgery to the new centre frees-up capacity at these other hospitals.
The proposal for the Elective Orthopaedic Centre was set out in a ‘decision making business case’ – and is summarised below.
You can find practical information about having surgery at the elective orthopaedic centre on the North West London University Healthcare NHS Trust website.
Our plans summarised
We have brought together much of our routine, inpatient orthopaedic surgery for the population of north west London in a purpose-designed centre of excellence at Central Middlesex Hospital.
- Why did we need to change?
- How have services changed?
- How does this work in practice?
- What benefits will be delivered?
- Equity
- Download the decision making business case
- Our approach to improving orthopaedic surgery
Why did we need to change?
- We need to reduce our waiting times - The Covid-19 pandemic has had a big impact on waiting times for planned care across the entire NHS. The proportion of people waiting more than 52 weeks for orthopaedic care has increased by more than a quarter during the pandemic.
- We need all our care to be consistently of the highest quality - While performance against national indicators for clinical outcomes and patient experience in north west London is amongst the best, for some measures in some trusts, there is a lot of unnecessary variance between us and much room for improvement.
- We need to make our care more patient focused - Patients are positive about the quality of our care and helpful staff, but report frustration with long waiting times between initial assessment and surgery or during appointments. Patients say they want more control over their care, and they want us to organise our care system so that it is clear and consistent.
- We need to help improve health and reduce health inequalities - Improving orthopaedic surgery would particularly help older patients and patients from more deprived backgrounds. Musculoskeletal (MSK) disorders are one of the most common long-term health conditions for the most deprived 20 per cent of the population.
- We need to be prepared for the future - If we do nothing, the number of people waiting for orthopaedic surgery in north west London will increase by almost a fifth by 2030. We also need to make the most of digital and other technological advances, without leaving anyone behind.
How have services changed?
The elective orthopaedic centre forms a key part of an improved care pathway for adults who need routine, planned orthopaedic procures such as knees and hip replacements. There are around 4,000 operations of this type in north west London each year. Evidence built over many years shows that when this type of surgery is done frequently, in a systematic way, there is an improvement in both quality and efficiency.
Outpatient care (including pre-operative assessment and post-operative rehabilitation and follow up) will continue to be provided as and where it is now. And day case and surgery for patients with complex needs will continue in the hospitals where they are provided currently too. You can see how this works in the maps below.
See previous provision of orthopaedic surgical care in north west London illustrated below:

See new provision of orthopaedic surgical care in north west London map illustration below:

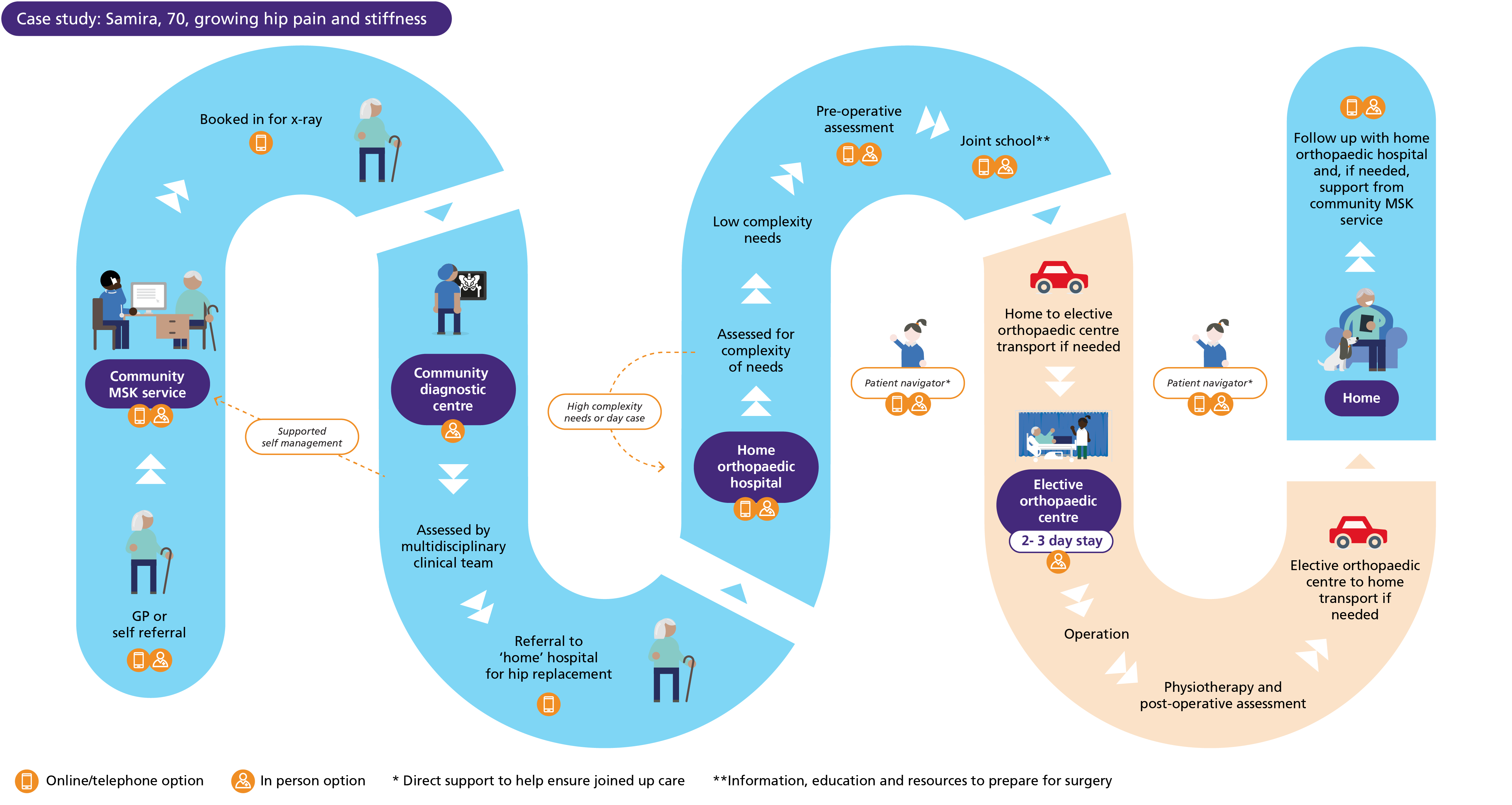
End-to-end care for patients who have their operation at the new centre continues to be the responsibility of the surgical team at their ‘home orthopaedic hospital’, with outpatient care provided locally or online. Patients only need to travel to Central Middlesex for their operation. Their ‘home orthopaedic hospital’ surgeons will carry out the operation at the elective orthopaedic centre with the support of a permanent, specialist team and our shared electronic patient record system. Door-to-door transport to and from the new centre is provided for patients who are unable to travel independently or via an existing patient transport scheme and who would otherwise encounter a long, complex or costly journey. Patients also have the support of a patient navigator to help guide them through the pathway and provide easy access to information, including about transport.
The clinical model has been developed with consideration of the whole patient pathway, including routes into and out of MSK community services. The integrated care board’s parallel re-procurement of community MSK services is providing additional opportunities to create a more joined-up experience for patients.
Patients are offered a single point of access to the most appropriate community-based treatment and, when specialist advice or care is needed, a consistent and timely onward referral to one of our ‘home’ orthopaedic hospitals. Post-surgery, the elective orthopaedic centre’s discharge hub acts as single point of referral to the eight north west London boroughs for patients who need social care, community rehabilitation or bedded rehabilitation.
How does this work in practice?
Here is an example of how the new pathway will work for Samira, 70, who is experiencing growing hip pain and stiffness.
What benefits will be delivered?
Care is of a consistently high quality, benefitting from latest best practice and research, provided by clinical teams that are highly skilled in their procedures – we expect to see a reduction in surgical complications and length of stay.
All orthopaedic surgery patients now have faster and fairer access to surgery, as we can use the capacity created in other north west London hospitals for surgical patients who have more complex needs and for other specialties.
Patients at the elective orthopaedic centre are much less likely to have their operation postponed due to emergency care pressures as the Central Middlesex is completely separated from emergency services.
The elective orthopaedic centre is extremely efficient, enabling more patients to be treated at a lower cost per operation.
Staff have more opportunities to develop their skills and experience.
Equity
We have put a strong focus on ensuring equity throughout the development of the Elective Orthopaedic Centre – we have used an integrated impact assessment, alongside our consultation feedback to identify key challenges and possible responses.
We know that people from black, Asian and other minority ethnic communities are less likely to seek orthopaedic surgery than other groups. We will be undertaking more detailed waiting list monitoring and improving communications, engagement and support.
We want to make the most of digital and other technological advances without leaving anyone behind. We are tackling this issue across all of our services and will roll out new responses to support the new clinical model, including tailored communications and face-to-face service options for patients who do not want – or are not able – to use digital platforms. We will also offer interested patients help with building and using their digital skills to support their health and healthcare.
Our approach to improving orthopaedic surgery
The North West London Elective Orthopaedic Centre began its phased opening, with three operating theatres, on the 4 December 2023. The centre moved to full capacity with five operating theatres in May 2024.
A formal opening event was held on the 13 May 2024.
Now, much of the routine, inpatient orthopaedic surgery for the population of north west London takes place in this purpose-designed, centre of excellence at Central Middlesex Hospital. The centre is expected to perform around 4,000 procedures each year.
The decision to open a new elective orthopaedic centre follows a public consultation, plus further feedback, review and scrutiny. The Full Business Case is available to view on this site along with other relevant documents.
Ongoing public engagement is central to the success of the new centre. We are gathering early insights and feedback on accessibility, information, signage and patient experience to ensure we pick up and respond to any issues that emerge during the phased opening.